How to take good Before and After pictures
When submitting your photos to Ellipse’s Before and After competition, it is best to use photos taken with a digital camera with high resolution. Even if you are taking pictures that are only going to be showed to the patient, a digital camera is the safe choice for taking before and after pictures.
Quick checklist before taking the photo:
___ Digital camera with high resolution
___ Hold the camera close to the treated area
___ Nothing in the background
___ Focus on the same area
___ Hold camera at the same angle
___ Same lighting /same time of day
___ No flash
The picture needs to be focused and usually it is better to move closer with the camera than to just use the zoom function. If your camera has a macro function (which looks like a tulip) it is a good idea to use it, but take a couple of practice shots on colleagues before using it on a patient.
It is important not to have anything in the background, which draws the attention away from the treatment result.
One of the most critical factors is to take the pictures of the same area and holding the camera in the same angle. This also helps the patient get a better grasp of the result. If there are markers on the skin, for example an untreated freckle, this can be used to line up the shot.
Another thing that makes the picture more believable is to take the picture in the same light. This can be done if you have a room or wall away from windows or direct light, and by taking the pictures around the same time during the day.
It is important not to use the flash from the camera, since light spot can appear in the picture and blur, or interfere with, the result.
During a treatment
Tips during the treatment
Every person in charge of a treatment has his or her own tips or tricks to give the patient the best result possible and to make the experience as comfortable as possible. We have gathered some of them here.
Wear eye protection
Make sure everyone in the treatment room wears eye protection – the patient, any students present and the operator.
Give the patient a stress ball
If the patient has a stress ball to squeeze during the treatment, this will reduce the feeling of discomfort
Another test shot
Even thought it is not the first time the patient is being treated, make sure to start out with a test shot based on the machines recommendations. Many things can cause a change in the patient’s sensitivity and a test shot will help the operator to find the proper settings every time.
Count backwards from three
Many patients benefit psychological from knowing when the shot will come. However some patients actively dislike this, so it is a good idea to discuss it with your patient before treating.
Right amount of gel
The amount should be sufficient to ensure that it does not dry out during the treatment, but not so great as to cause a build-up of gel on the side of the crystal light guide. Note that the gel should not contain air bubbles.
Place the light guide perpendicular to the skin
This ensures that the largest amount of the crystal is in contact with the gel and therefore that the maximum amount of light energy penetrates the skin surface. It also reduces the risk of leaving untreated strips on the skin.
Keep the sides of the light guide free from gel
This reduces the risk of light being emitted from the side of the light guide instead of the bottom of it. A build-up of gel on the sides can result in the patient getting “zebra stripes” after treatment.
Do not slide the applicator across the treatment area
This offers two advantages. You avoid a build-up of optical coupling gel on the side of the applicator and you leave a “footprint” of the area you have treated in the gel. This makes placing the subsequent shots easier and avoids the risk of either missing or double-treating an area of the skin.
Start in the area that is least sensitive to pain
On the face, this is far from the nose and upper lip. More generally areas further away from bone are less sensitive
Encourage patients to ask for a few seconds break in treatment
Most often, intense pulsed light treatment is selective treatment and the experience should be made as comfortable as possible for the patient.
Immediately before a treatment
Things to remember
When the patient has arrived for his or her treatment there are several things to do, before starting the treatment itself.
- Remove patient make-up
- Take before pictures
- Shave the treatment area if needed
- Mark the border of treatment area
- Determine the skin type and suntan
First of all, remove the patient’s make-up:
Cosmetics can disguise the true appearance of the skin, and can also absorb some of the light needed to carry out the treatment. This can lead either to an inefficient treatment or an increased risk of side effects.
Take before pictures of the treatment area:
The main purpose is to show the progress of the treatment to the patient (as a series of before and after treatment). And if you ask for the patient’s permission, it’s possible to use the pictures in Ellipse B&A competitions, or to show other patients. Our next blog will give a little more detail on how this can be done.
Shave the treatment area (if required)
Shave or trim the hair and always remember to remove the hair after the area has been shaved. Hair above the skin surface will absorb energy from the applicator and can burn into the crystal light guide (damaging the applicator, and leaving marks on the patient) or can burn onto the skin surface, causing pain or skin burns during treatment.
Some hair removal patients prefer to shave the area themselves, and it can be a good idea for them to do this, a few hours before the treatment. If they cut themselves shaving, the few hours interval gives time for the area to repair, and all blood (which will absorb the light) to be removed from the skin surface. But remember that the patient should shave not longer than 1 day before treatment, and should leave a patch of hair so that you can see the hair thickness.
Mark the border of the treatment area
If you are doing full face rejuvenation, or treating a blood vessel, this is obviously not necessary, but for hair removal mark the border with a red pen or a white wax pencil. Do not use other colours, as they will absorb the light and can cause a skin burn.
Determine the skin type and degree of suntan
Use the Fitzpatrick scale to determine the skin type, furthermore determine the degree of suntan, the size and colour of the target. Enter this into your Ellipse machine and it will supply you with treatment settings.
If you want to read more about using the Fitzpatrick scale to determine the skin type you can do it here.
Achieving Maximum Onychomycosis Clearance Rates
As well as our own multi-centre Clinical Study, Ellipse has undertaken a literature review, taken expert opinion from the dermatologists we work with, and picked up information from conferences around the world. Based on this, we are pleased to offer this short professional guide to treatments, and how to get the best possible clearance result. A patient guide is also available.
Background – When we introduced the treatment , we were quite clear that the treatment is ”Temporary increase of clear nail in patients with onychomycosis”. This is also the approved wording of the US Food and Drug Administration (FDA). In other words, this is not a vaccine guaranteeing permanent freedom from nail fungus. An individual patient may have nail fungus because of injury to the nail or because of health or environmental factors – all of which make reinfection possible. This is equally true if the treatment is based on medication or on light, and in both cases health and lifestyle changes can help to reduce the risk of reinfection. A list of recommendations to patients is shown in the patient guide.
The sub-millisecond pulse is better. Our original study compared a 35ms pulse with a sub-millisecond one, and the 12 month follow-up clearly shows the superiority of the shorter pulse.
Ellipse has had no negative feedback about the efficacy of our treatment, but various national conferences have included comments that with other light-based treatments, reinfection occurs before the whole nail is clear. We would therefore make the following suggestions to maximize the treatment effect:
- If nails are thick, file them down to 1-1.5mm thickness before laser treatment is performed.
- Perform 4-5 treatments with 1-3 weeks interval to maximize the destruction of the fungus.
- Use 4 consecutive passes on each nail, before changing to the next nail. Treat a fifth pass as optional.
- Use a fluence of at least 16J/cm2. Higher fluence will improve the result, so increase up to 22 J/cm2, if the patient can tolerate it.
- Undertake a 3 month post treatment follow up. If in doubt that all fungus has disappeared, perform an additional treatment.
- Ask the patient to come for a check-up every 6 months until all nails have completely recovered and perform an additional treatment until complete clearance is achieved.
- Laser treatment might benefit from the combination of home treatment with a water based topical nail lacquer such as Onytec or Ciclopoli, with 8% ciclopirox(i) (ii) , as the active compound, applied to the nail in accordance with manufacturer’s instructions.
- Ensure that the patient is fully aware of his or her role in preventing reoccurrence.
- If there appears to be no improvement after treatment, check that the patient does have onychomycosis and not another disease such as psoriasis.
(i) Monti D, Tampucci S, Chetoni P, Burgalassi S, Mailland F. Ciclopirox vs amorolfine: in vitro penetration into and permeation through human healthy nails of commercial nail lacquers. J Drugs Dermatol. 2014 Feb;13(2):143-7
(ii) Togni G, Mailland F. Antifungal activity, experimental infections and nail permeation of an innovative ciclopirox nail lacquer based on a water-soluble biopolymer. J Drugs Dermatol. 2010 May;9(5):525-30.
If you want to download the Whitepaper click here.
If you want to download the Patient Guide click here.
Onychomycosis (Nail Fungus) – A NEW Ellipse treatment
October 2013 saw the international launch of the new Ellipse Nd:YAG treatment of onychomycosis (nail fungus). The launch took place at EADV 2013 in Istanbul.
The treatment
Ellipse laser treatment of Onychomycosis offers a quick, painless and effective treatment. Quick: because of a new sub-millisecond pulse, and a high repetition rate, it is possible to treat 10 nails in 10 minutes. Painless: patients were asked to grade the pain on a level from 0-10, and gave an average score of 0.25! This is because of the short pulse used (which seems to confuse the nerves that would send pain messages) and even more because the Ellipse has SoftCool technology that blows a constant stream of cool air over the area being treated. Effective: in the study 79% of patients saw an improvement in their nails, shown as an area of clear nail growth. Because nails (especially toe nails) grow slowly, this is not an overnight effect, but a process which can take a year to fully resolve.
Treatment is available on the Ellipse MultiFlex+, and are simple for both the patient and the operator. The nail must be clear of polish, and cut short. Treatment uses a standard pulse and standard energy and the laser moves across to cover the whole nail including the nail folds, with a 50% overlap. Five passes are made over each complete nail.
A pass-counter ensures that nails can receive the full five passes, even in the busiest clinics.
The disease
Onychomycosis is unbelievably common (estimates vary but between 2% and 8% of the world population is affected). It affects mainly adults, and the chances of developing it increase with age (although adults who swim or run are at increased risk, because of infection from puddles in communal showers, or trauma to the toes when running). The chance of an individual developing the condition is 20%. A study – the Achilles project – across Europe and East Asia (China, Taiwan and South Korea) showed that more than 1 person in 4 visiting his family doctor had the condition, and this figure rose to more than 1 in 3 if he was seeing the doctor for anything involving feet.
Onychomycosis can be caused by several different fungi, and the appearance of nails can vary, but typically nails are thick and discoloured (white, black, yellow or green). The nail may be brittle, broken or even totally missing nails; there may be white or yellow patches on the nail-bed, and surrounding skin may be inflamed, painful or scaly.
Other treatments
Various other treatment modalities exist (including various home remedies), but the main options are
- to use a topical anti-fungal nail-paint available from a pharmacist,
- to use a stronger (prescription) anti-fungal paint following a doctor’s visit.
- to use a course of systemic (taken by mouth) anti-fungal drugs.
Both the prescription paints and anti-fungal drugs carry a significant risk of side effects, which can be unpleasant. And they do not always work: the nail-paints have an average success rate of below 30% (as low as 15% on toe nails) while the various studies of oral medication shows success to be from 50-70% at best. A further complication is the long treatment time, typically between 3 to 11 months, and sometimes a variable treatment pattern where the patient takes them for a while, rests and takes them again. This can cause certain patients to forget to comply with the instructions.
By comparison, Ellipse laser treatment is a series of 3 short treatments, with no side effects and no pain, offering a greater success rate than medication without the side effects.
Further information
Click on the Link to download a copy of our White Paper, or Information Sheet, or Patient Leaflet.
Click on this Link to see our treatment video on YouTube
Ellipse Acne and Wrinkle Treatments: The Clinical Evidence
Ellipse Intense Pulsed Light Treatments of Acne and Wrinkles
A quick introduction:
Ellipse acne treatment works in combination with a medication called adapalene (marketed as Redap® or Differin® gel or cream). There is a also considerable clinical evidence that using light from the Ellipse PR+ or PL+ applicator, together with a 5-ALA photosensitizer produces a significant improvement in Acne, (or a great-enough improvement in collagen production to reduce fine lines and wrinkles). Using a light source together with a photosensitizer, is known as Photodynamic Therapy (PDT).
So we have to add a legal note here. Ellipse is cleared as a light source, but there are currently no photosensitizers approved for treating acne nor improvement of fine lines. For regulatory approval status, please see “Instructions for use” or contact Ellipse A/S. Information is included not as an endorsement of a treatment for which Ellipse does not have regulatory approval of, but to raise awareness of the research.
Acne: The clinical evidence (Ellipse I2PL)
This quite large study (116 Chinese patients) showed 85% had a 30% improvement in acne and over 40% had a 60% improvement – using light alone – from 5 treatments.
A split faced study comparing use of a standard acne medication alone (benzoyl peroxide gel) with a combination treatment of benzoyl peroxide gel and Ellipse Intense Pulsed Light. The study found that use of Ellipse Intense Pulsed Light gave improvements in acne red macules, irregular pigmentation, and skin tone in Korean acne patients.
Acne: The clinical evidence (Ellipse I2PL in combination with 5-ALA)
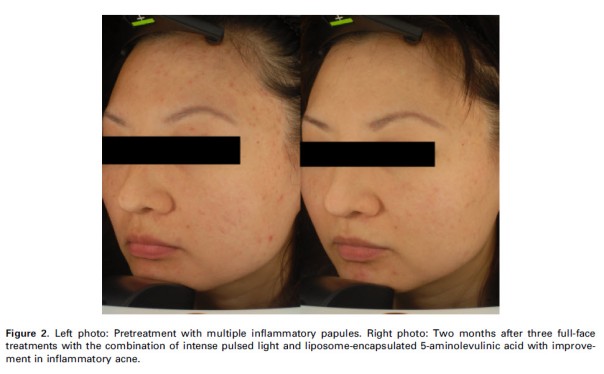
A pilot study looking at acne in an Asian (Hong Kong) population. Results were encouraging showing mean reductions in inflammatory lesions of 52% at 1 month and 65% at 6 months after treatment, and also a drop in the level of sebum production on the forehead (lasting approx. 1 month). The treatment protocol was subsequently altered to include a waiting period between application of the PhotoSpray and start of light treatment.
Another encouraging Asian study, this time from Korea. The mean reduction in acne grade at the end of the treatment was 43.2%. 69.2% of patients reported improvements in subjective skin oiliness (sebum production). The study also reveals PhotoSpray is better tolerated by Asian patients than the alternative (higher-concentration) ALA sources, causing no side effects.
One of the first published studies, and one which showed conclusively that 0.5% ALA is selectively absorbed (and converted) in the sebaceous glands of patients with acne, and also that the light used in the treatment causes the converted Protoporphyrin IX to be photo-bleached (used-up).

A) Before treatment; B) concentration of PpIX in the acne nodule after 1 hour spraying with PhotoSpray C) lower concentration after light treatment
Both the clearance rates, and the before and after pictures are impressive, as is the fact that there were no adverse effects from treatment.

Left: Before Li-PDT-PC. Right: After 6 Li-PDT-PC treatments in 6 months (improvement 90%). No side effects. No effect from previous treatment with cyproteron ⁄ ethinylestradiol and systemic minocycline.
It is worth noting that the study assessed the efficacy and the safety of PDT using 5-ALA 0.5% in liposomal spray and intense pulsed light (IPL) in combination with topical peeling agents (Li-PDT-PC).
Wrinkle Reduction: The clinical evidence (Ellipse I2PL in combination with 5-ALA)
A study showing statistically significant improvements in periorbital and nasolabial wrinkles. The average overall improvement was greater for periorbital than for nasolabial wrinkles. No side effects were observed during and after treatment. The degree of overall improvement was scored as excellent by 47% of the volunteers.
Ellipse Vascular Treatments: The Clinical Proof
Ellipse Intense Pulsed Light Treatments
A quick definition:
Vascular treatments are treatments of blood vessels, and use of laser and intense pulsed light tends to be restricted to veins, venules (smaller vessels that link veins to capillaries) and capillaries (the smallest blood vessels). The location, structure and rapid flow of blood in arteries and the smaller arterioles makes them unsuitable for light based treatment. Ellipse has two different Intense Pulsed Light applicators, the PR+ (with a waveband from 530-750nm and the VL+ 555-950nm, which allows treatments of vessels at different depths in the skin, as well as an Nd:YAG laser (1064nm). Choosing the correct tool enables Ellipse users to treat vessels of many different sizes, and therefore treatment of many different vascular problems. As always, it is easy to claim success, but Ellipse has a considerable amount of proof – enough to be considered the new gold standard for vascular treatments.
The clinical proof:
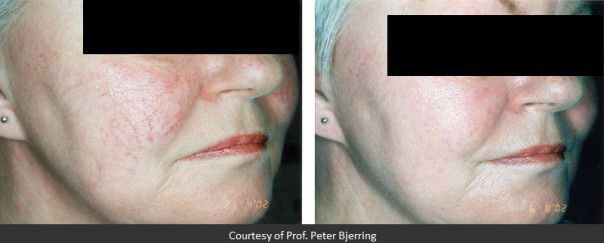
Intense pulsed light source for the treatment of facial telangiectasias. P. Bjerring et al. (J Cosmetic & Laser Ther 2001; 3: 169 – 173)
The first Ellipse vascular paper, and one which showed excellent clinical results (All patients showed some improvement, 83% showed a 50% or greater improvement and 67% showed a 75% or greater improvement). Not only that the study showed that the risk of side effects of treatment was lower than with laser, and that no skin cooling was required.
As a quick background information, no treatment has 100% success rates. This study looked at treatment of patients who had previously not responded to the other “state of the art” treatment – Pulsed Dye Laser – and found that many (all those treated outside a certain central area of the face), called the V2 area) responded to Ellipse Intense Pulsed Light.
The study took a group of German patients and treated part of the PWS with a reputable pulsed dye laser, and part with Ellipse Intense Pulsed Light. Results showed 85% of the treated PWS responded with clearing. Better clearing by PDL was seen in 13%, whereas IPL was superior in 42%. No differences in clearing were recorded in 31%, and concluded ” These preliminary data suggest the IPL technology as a superior treatment option for PWS”.
The superiority of Ellipse Intense Pulsed Light over Pulsed Dye laser was confirmed in a larger study “Comparison of intense pulsed light (IPL) and pulsed dye laser (PDL) in port-wine stain treatment. Michael Drosner et al. (Medical Laser Application 23 (2008) 133 – 140)” and separately by “Split-face comparison of intense pulsed light with short- and long-pulsed dye lasers for the treatment of port-wine stains. Philipp Babilas et al. (Lasers in Surgery and Medicine 42: 720- 727, 2010)”
Early treatment of haemangioma in childhood using IPL. M. Drosner (EADV, 16-24 May, 2007)
An important study that found good results in treatment of newborn children with haemangiomas. However, this has partly been overtaken by use of the drug propranolol.
A study which showed 90% clearance in telangiectasias without the risks associated with using Pulsed Dye Laser .
It is often said that clinical studies use only a few patients; here is a study on 238 Chinese patients that found all showed improvement of at least 30% from 1-3 treatments (over 40% showed at least 60% improvement). The study also reported an improvement in wrinkles following treatment.
Ellipse Nd:YAG treatments
Of course, it is possible to treat certain vessels with Ellipse Nd:YAG instead of Intense Pulsed Light. Leg vessels respond much better to the longer wavelength of the Nd:YAG, but the Nd:YAG can also be used for difficult telangiectasias on the face.
Five men and seven women were enrolled (aged 43 ± 5.8 years). Total clearance of vessels was 78.3%. The number of vessels in diameter of 0.1 mm was reduced by 61.1% and that of vessels in diameter of 0.2–0.3 mm decreased by 92.2% on the average at 12-week follow-up. Eleven of 12 patients were very satisfied with the clinical results. One patient rated as ‘satisfied’ due to hyperpigmentation after the treatment, which improved at 2-week follow-up.
Ellipse Rejuvenation: The clinical proof
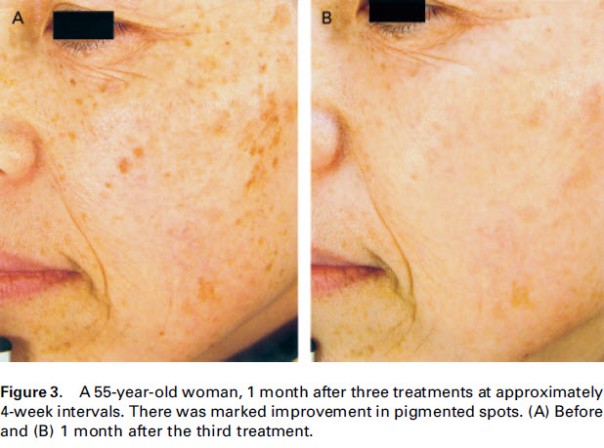
Ellipse Rejuvenation treatments (Skin Rejuvenation or Photorejuvenation depending on the applicator used) are treatments to improve sun damaged skin – which either presents as redness (leading eventually to formation of larger blood vessels) or as areas of dyspigmentation, and eventually age spots (also called liver spots and medically called solar lentigines). In the US, the term rejuvenation is not allowed (there it is officially referred to as redness and pigmentation). But system operators and patients as always deserve to know that the treatments they offer or receive work. The list below shows some of the clinical proof provided by Ellipse.
The first study, and an important one that should widespread success, but also showed that in European skin, on applicator used , the VL-2 (now remodelled as the VL+) produced better results on pigment, while the PR (now PR+) achieved better results on redness. The study also reported that despite using less energy, success with Ellipse required fewer treatments than than with other Intense Pulsed Light devices..
A fascinating study that shows not only high patient satisfaction, but highlighted a condition called hidden melasma, rare in Europe but more common in Asia, that had the potential to be impacted by treatment. Even more interesting, the study showed some ability to lighten the skin of the patient
An important study showing that Ellipse treatments not only had a positive result on redness and pigment but also on skin texture
Another study showing good results, but also finding that vascular treatments on Asian skin were better using the VL-2/VL+ applicator, because of the slightly thicker epidermis
Ellipse Hair Removal: the clinical proof
Hair Removal is the basis for many clients seeking Intense Pulsed Light treatment. For the clinic owning the equipment, it is equally important to know that the system used removes hair, and that it stays away.
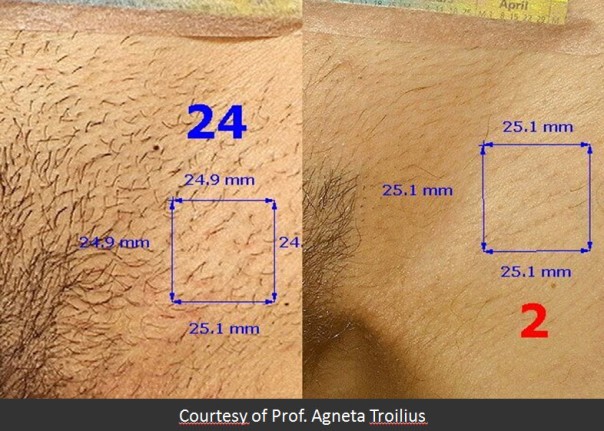
The first published study by Ellipse investigated the bikini line hair of 10 Swedish patients. A hair count was made before, 4 months (1 hair cycle) after and 8 months (2 hair cycles after) 4 treatments (1 month between treatments).
The study showed hair reduction of 75% at 4 months and 80% at 8 months
In 2000, use of ruby laser for hair removal was the norm, and this study found that 93.5% of patients treated with Ellipse I2PL achieved measurable hair loss, compared to only 55% with the ruby laser. Figures for both systems were lower than would now be expected, as treatment parameters and intervals have evolved in the subsequent 13 years.
An interesting German study that compared Ellipse 2nd generation Intense Pulsed Light with a first generation system (ie the effect of dual mode filtering) and with Diode and Alexandrite lasers. Various body sites were treated with each system. “The best results were obtained with the second generation IPL system Ellipse”
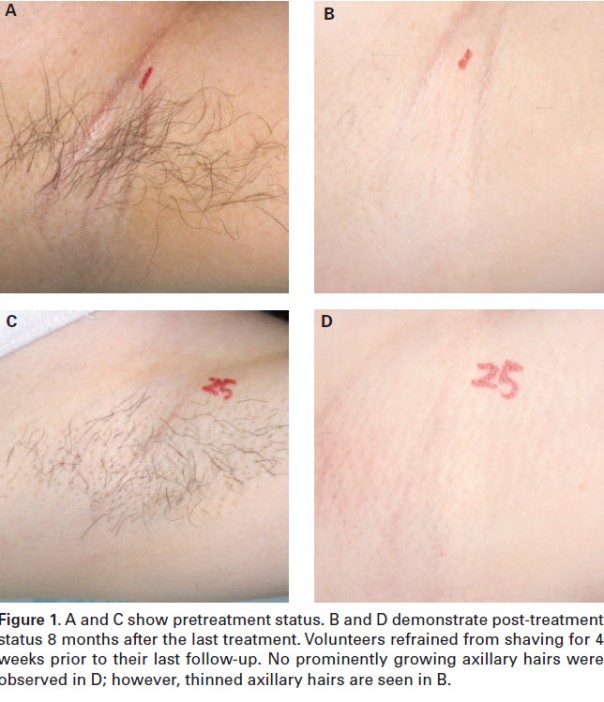
A Korean study comparing the HR and HR-D applicators when treating axilla. The HR-D gave an average clearance of 83%, with no side effects.
A huge study of 365 patients, that showed the HR applicator to remove and average of 96% of hair after 3-7 treatments.
An interesting Swedish study that looked at hair removal in various groups of “problem” patients, transsexuals, those with hormone problems (including Polycystic Ovary Syndrome – PCOS – and those whose hirsutism was caused by medication. The number of treatments required to get results is naturally higher, but the study concluded that (Ellipse) IPL was equally as effective in patients with hormonal problems as those without.
Two papers on a very long term follow-up study (5-9 years after treatment) ended, that found only very modest regrowth after this time, and concluded that treatment could be considered as permanent hair removal.
The image shows a clearance of 63%, 9 years after the end of treatments.



















You must be logged in to post a comment.